Unfortunately, approximately 60% of Australian women and 75% of Australian men were reported to be overweight or obese in 2017-18 (Australian Institute of Health & Welfare, 2020). This is an increasing concern for the Australian population.
Studies have found that individuals who are overweight or obese may experience challenges when it comes to fertility (Silvestris et al. 2018; Zain et al. 2008). These challenges may include menstrual dysfunction and lack of ovulation, or compromised fertility in women who are still ovulating. Additionally, being overweight or obese during pregnancy can increase complication risks (Pandey et al. 2010).
Studies have shown that obesity increases time to conception and for every BMI unit above 29kgm2, fertility decreases by ~4% (Van der Steeg et al. 2007).
Obesity and being overweight is also associated with polycystic ovarian syndrome (PCOS) which is a hormonal condition affecting between 6-10% of women of reproductive age and often develops during adolescence (Barber et al. 2021).
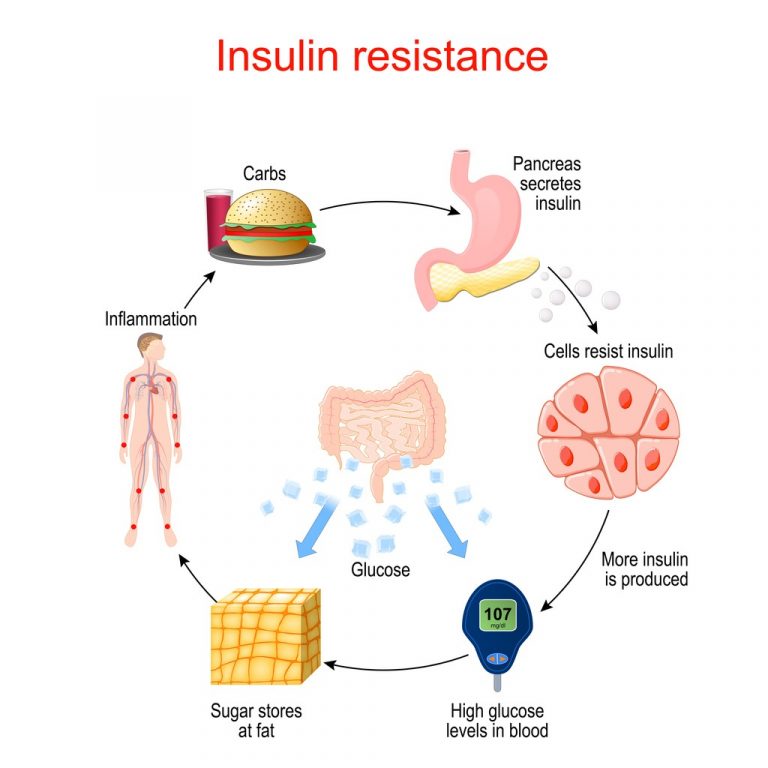
PCOS can disrupt the balance of a hormone called insulin and cause insulin resistance (Goodarzi, et al 2011). Insulin resistance can cause weight gain and increased appetite, which in turn may alter hormonal levels (androgens and oestrogen) which ultimately may affect egg quality and the frequency of eggs being released from the ovaries.
How does losing weight and bariatric surgery change or improve fertility?
Research has shown that bariatric surgery and significant weight loss can improve fertility for both women and men (Moxthe, et al 2020). These improvements to your fertility mean that conceiving a child is often much easier following bariatric surgery.
Studies report that women who suffer irregular menstrual cycles and/or anovulation (lack of ovulation) may in fact experience re-balancing of their hormones and as such, restoration of regular ovulation and menstrual cycle in as little as 12 months following weight loss surgery (Moxthe, et al 2020). This includes significant improvement in PCOS symptoms including reduction in HbA1c %, reduction in insulin resistance, resolution of normal menstrual cycles, and significant improvement of hirsutism, and androgen profiles (Malik et al. 2012).
For men, being significantly overweight is associated with increased circulating female sex hormone (oestrogen) and reduced male sex hormone (testosterone). Weight loss and bariatric surgery helps to reverse the oestrogen and testosterone levels, returning the hormonal balance to normal. Sperm count and sperm quality may also improve after bariatric surgery.
Which nutrients need to be monitored after weight loss surgery when you are trying to conceive, and why?
As bariatric surgery involves changing the structure of your digestive system, the body struggles to absorb nutrients as it once did. So it is important to understand it is harder to meet your nutritional needs through diet alone, and you will need vitamin supplementation. Common nutrient deficiencies in patients who have undergone bariatric surgery include iron, B vitamins (B12 and folate), calcium, vitamin D, zinc and essential fatty acids (omega-3).
Iron: Iron is an essential nutrient and cofactor for the synthesis of haemoglobin which is involved with oxygen transport, respiration, growth, gene regulation and functioning of iron-dependent enzymes (Mousa et al. 2019). Iron deficiency is most commonly seen after bariatric surgery (Slater et al. 2017). Women of reproductive age are most at risk of iron deficiency due to menstrual losses and low intake of absorbable iron (e.g. red meat, poultry and fish) (Mousa et al. 2019) (Slater et al. 2017).
The current guidelines state that patients who have undergone bariatric surgery should monitor iron status routinely and supplement with 45-60 mg of elemental iron, and this may be increased as required for menstruating women (Slater et al. 2017). Intake of vitamin C supplements will help increase iron absorption.
Vitamin B12: Vitamin B12 is an essential coenzyme for the function and development of brain and nerve cells, healthy formation of red blood cells and DNA synthesis (National Institute of Health 2021). Vitamin B12 deficiency is quite common, occurring in over 50% of pregnancies post-surgery due to the reduced availability of intrinsic factor in the stomach, and malabsorption (Slater et al. 2017). You may need additional sublingual B12 supplementation or intramuscular injections.
Folate: Folate is essential in DNA synthesis (Mousa et al. 2019). Adequate folate is needed for women who plan to get pregnant regardless of whether you have had bariatric surgery or not. Folate requirements are increased during the conception period and pregnancy to prevent neural tube defects in the baby (Mousa et al. 2019). Although folate deficiency may occur after bariatric surgery, it is uncommon since folate can be absorbed in other parts of the small intestine (Slater et al. 2017). Studies indicate it is advisable to take up to 5 mg of folic acid daily following bariatric surgery (Slater et al. 2017).
*Please check with your healthcare provider which form of folate (not all “folic acid” is the same) is best suited to your needs. In most cases, it is best to consume the activated form of folate, which is not “folic acid”.
Calcium: Calcium is an essential nutrient for bone mineralisation and a key component for maintaining cell membranes (Mousa et al. 2019). Although the primary source of calcium is dietary, the recommended targets are nearly impossible to achieve post weight loss surgery without supplementation. Requirements are between 1200-1500 mg daily of calcium citrate with vitamin D3 and are higher for gastric bypass (Xanthakos 2009). If possible, do not take your iron and calcium supplements together, as neither will be absorbed properly.
Vitamin D: Vitamin D is necessary to enhance calcium absorption and maintain bone strength (Mousa et al. 2019; Slater et al. 2017). It is estimated that between 40-100% of pregnant women are vitamin D deficient worldwide (Slater et al. 2017). Vitamin D deficiency is associated with rickets in young children, babies’ growth restriction, preeclampsia and possibly lowered immunity (Slater et al. 2017). Routine supplementation of a minimum of 1000 IU daily is recommended following bariatric surgery.
Zinc: Zinc has many important roles in our body, such as protein synthesis, cellular division, gene expression, wound healing, vision, and brain and immune function (Mousa et al. 2019). Recent research has found that many patients booked for bariatric surgery were zinc deficient on their preoperative blood tests (Soheilipour et al. 2021). Zinc deficiency in pregnancy is associated with impaired immunity, prolonged labour, preterm and post-term births, intrauterine growth restriction and high blood pressure (Mousa et al. 2019).
Omega-3: Consumption of a diet rich in omega-3 can improve egg quality and help preserve ovarian reserve, particularly in older mothers (Nehra et al. 2012). Adequate DHA consumption is positively associated with the development of the baby’s brain and eye (Mousa et al. 2019).

Weight gain during pregnancy after bariatric surgery – how much is recommended?
How much weight gain is okay after bariatric surgery?
It may feel daunting to think about weight regain during pregnancy after you’ve worked SO hard to lose weight. Some weight gain is expected and needed during pregnancy to support a healthy growing baby!
The amount of recommended weight gain will depend on your pre-pregnancy BMI.
It has long been said that “you are eating for two when pregnant”, but this is actually not the case. There are recommended amounts of weight gain for each trimester, with the first trimester occasionally seeing a weight loss for those experiencing severe morning sickness. There are minimal energy requirement increases in the first trimester and the most important thing is to ensure you are taking a prenatal vitamin daily that has been well matched to your needs by an experienced dietitian. Certain extra nutrients will be required for pregnant mothers with a history of bariatric surgery.
The second and trimester are when most weight should be gained during pregnancy to support your growing baby. What you eat during pregnancy, and getting enough of the essential nutrients, is very important for your baby’s long term health.
If you have had weight loss surgery and would like advice on how much weight gain is advisable during pregnancy to reduce risks to you and your baby, and to avoid unnecessary weight gain, please don’t hesitate to reach out for an individualised weight management plan and monitoring during this crucial time.