The decision to go ahead with bariatric surgery is a life-changing decision for most.
As a clinician who is passionate about helping people achieve and live their best life, I wanted to share with you the inside scoop on how to ensure your bariatric surgery is a SUCCESS!
Remember, “your surgeon is the one who removes / bypasses your stomach, but you’re the one in control of your life!”

Eating is a behaviour!
Did you know that we eat for other reasons despite just being hungry? We eat for emotional, social and behavioural reasons. We make hundreds of food decisions each day that are influenced by a variety of personal, social, cultural, environmental and economic factors. Additionally, eating is a fundamentally rewarding behaviour, therefore it can be closely linked to mood and emotions (Vögele and Gibson, 2010).
So, it’s not just about the immediate problem and wanting to lose weight, but it’s being prepared to address reasons as to why and how you got here – and what you want your future to look like too.
In my career I’ve seen too many people put weight back on after taking the brave, difficult step to get surgery and I want to be part of the solution. I help people understand these and learn to use new eating methods to retrain the brain to recognise and work on these areas.
If you have any questions about weight loss surgery, weight loss options to try before making the decision on surgery, or how I can help you, please don’t hesitate to get in touch.
Is there anything I need to do before weight loss surgery?
Yes. A ‘very low-calorie diet’ (VLCD), or a liver reduction diet (LRD), must be followed in the 2 weeks prior to surgery (Colles SL, et al. 2006). The VLCD usually consists of 600-800 calories per day which will shrink the liver size to assist keyhole (laparoscopic) surgery, reduce the risk of operative complications (Anderin et al, 2015) and is an excellent start to your weight loss journey (Bettini S, et al. 2020). You can expect anywhere from 2-6kg (or more if you are starting from a higher weight) weight loss in the 2 week period if the VLCD is adhered to strictly (Sivakumar J, et al. 2020).
Meal replacement shakes, bars or soups such as Optifast or Formulite – which are nutritionally complete in a certain amount and high-protein but low-calorie – are usually the best option. Your dietitian will advise what is the most suitable option for you, how many shakes, bars or soups you need each day and whether you need a daily multivitamin as well. It is important when following a VLCD to ensure you have checked with your surgeon or doctor beforehand regarding any medications you are taking. It is also very important to ensure you are adequately hydrated with up to 3L water per day whilst following the VLCD.
What does a post-bariatric surgery diet look like?
The post-op diet changes a lot in the first two months depending on how you are tolerating things. The dietary recommendations are based on gradual progression of food texture over 1 to 2 months.
Usually immediately after surgery you will be allowed to sip clear fluids like water and broth. Soon after, you will progress to a full liquid diet to ensure nourishing, high-protein fluids are consumed as soon as possible. It is common to stay on the full liquid diet phase for approximately 2 weeks after surgery whilst the swelling starts to settle and you get used to regularly sipping fluids and not gulping (Tabesh et al, 2019).
Around the 2 weeks post-op mark, your Dietitian or surgeon will give you the all clear to move to a puree-texture diet. If you’ve been having trouble on the full liquid diet, then you may be asked to remain on liquids for a while longer. After you have progressed through the fluid phase you will move on to puree textured foods, this phase is a bit like the baby-food phase! Although, it can be made a lot more interesting!
After 2 weeks on puree foods, the next step is soft foods which includes boiled eggs, moist minced-meat, soft poached fish, cottage cheese, rolled oats made with high protein milk and then normal consistency diet. The dietary progression from full liquid diet to normal consistency food can take between 6 to 8 weeks (Kulik et al, 2010) (Tabesh et al, 2019).
After any weight-loss-surgery, it is recommended that all foods are always thoroughly chewed to minimise any risk of problems, meals are eaten slowly and fluids are drunk separately either 15 minutes before or 30 minutes after a meal. It is important to work with your dietitian, especially during the early phases, to ensure you are consuming enough protein each day, and figure out ways to achieve this if you are struggling (Kulik et al, 2010).

Will I lose my hair?
Hair loss after weight loss surgery and/or with PCOS, thyroid conditions or post-partum are all too common and unpleasant. 😥
This can happen in the first six months after surgery with extreme weight loss. It is usually related to the stress of losing so much weight, and the hair follicles go to sleep.
However, it is less likely to happen if you meet your daily protein goal (this will vary and is individualised) and take your recommended multivitamins as directed by the dietitian.
Mini-gastric bypass or gastric bypass at greater risk of all nutritional deficiencies due to the malabsorptive process of the surgery. All weight loss surgeries restrict portion size, so it’s important to hit your nutrition goals at all meals and snacks. 🍣🍓🥑🥕🍆🍳
After doing some thorough research, the main nutrient players in hair loss are iron, vitamin D and zinc which support growth of the hair follicle 💁🏼♀️ Deficiencies of niacin (B3), biotin (B7) and B12 (identified on blood test) are also connected to hair loss.
A severe reduction in carbohydrate intake may also result in hair loss, so it is important for your hair, and your metabolism, to reintroduce carbs once you are tolerating your liquids post-op. Choosing high-quality carbs only! 😁
Too much of certain vitamins like vitamin A or selenium (found in vitamin supplements) have been shown to cause hair loss, so make sure you know what multivitamins you are taking, and if they are right for you!
Bloods tests for vitamin D and zinc levels which are considered “normal” by your GP, might not be right for you, especially post weight loss surgery. Ranges vary widely across different pathology sites. Check with your weight loss surgery dietitian if you’re concerned.
A low intake of essential fatty acids (omega-3s) may contribute to poor hair growth and hormone function. Omega-3s are a non-negotiable. If you don’t eat salmon, sardines, mackerel, herring or anchovies, invest in a high-quality omega-3 supplement!
My top 3 foods for hair support are red meat 🥩, oily fish 🐠 and eggs 🥚!
Fortunately, hair loss will usually resolve on its own! Nutrient deficiencies will need to be tested if hair loss continues past six months.
Will my appetite return?
Having weight loss surgery doesn’t mean that you will never be hungry again… You might start to feel hungry 6-12 months after surgery or you may not ever feel hungry again and forget to eat, which is also a problem! It is really individual and varies from person to person.
Hunger is your body’s way of telling you that it needs fuel so it’s normal (even after surgery). Sometimes you’ll learn that you’re getting the hunger symptoms but it’s not the same as before e.g. there may be a gurgling in the stomach rather than the usual growling, or you may feel an empty feeling. If you are feeling light headed, dizzy, faint, weak then likely if you haven’t eaten or enough fluids – it is time to eat or hydrate.
If you find your appetite is out of whack, for example, maybe you don’t have an appetite, or maybe you have feelings of extreme hunger, here are some questions you can ask yourself that might help:
- Am I hitting my protein goals?
- Am I having enough fibre with each meal?
- Am I really stressed or having poor sleep?
- Am I moving my body each day?
- What is my fluid intake like? Am I having at least 1.5L minimum water intake each day?
Why is exercise an important part of the puzzle?
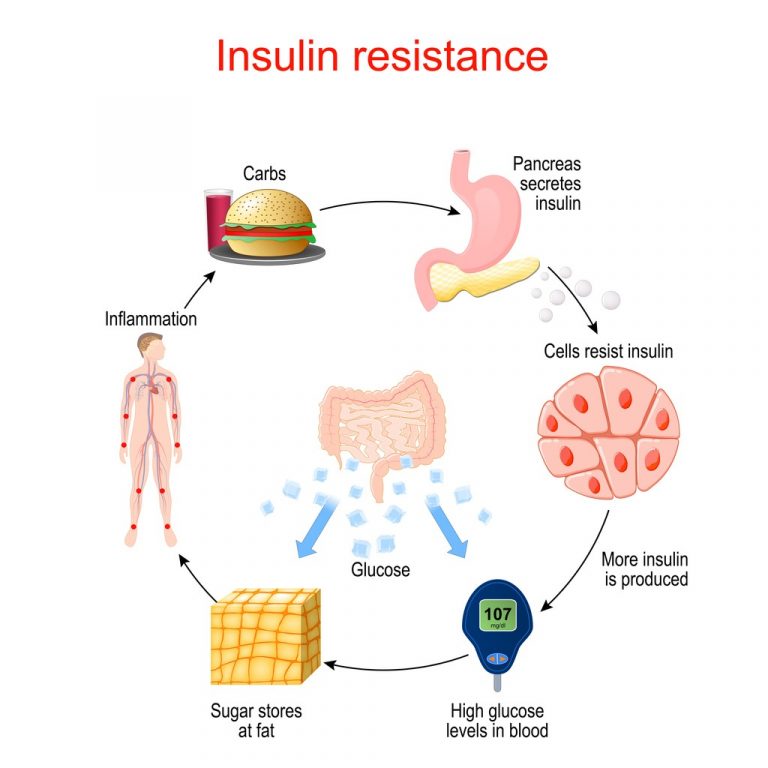
Physical activity not only plays an important role in preventing chronic diseases like diabetes, heart disease and obesity, but it also reduces the risk of death from various chronic diseases (Warburton et al, 2006). Exercise is a vital part of any weight loss program and enhances overall weight loss, assists with maintenance of ideal body weight and helps prevent weight regain. Aerobic exercise is particularly effective at reducing visceral adipose tissue which is strongly linked to insulin resistance and type 2 diabetes (Goedeckce et al, 2014).
One study found that participation in physical exercise is the single strongest predictor in weight loss the year following sleeve gastrectomy (Kessler et al, 2020). It can also help reduce the risk of recurrence of comorbidities and weight regain, 10+ years after bariatric surgery (Adams et al, 2017).
Unfortunately, there is no specific physical activity guideline for prescription of exercise before or after bariatric surgery. However, based on the general guidelines at least 150min/week of moderate to vigorous exercise (walking at a brisk pace, sports training, vigorously vacuuming) or 10,000 steps per day is recommended for improving general health. It increases to 150 – 200min/week or expending 1200 – 2000kcal/week (through exercise) for preventing weight regain and up to 300min per week for weight maintenance after weight loss.
When to start physical activity after bariatric surgery?
Any abdominal exercises should be avoided for the first 8-12 weeks after surgery to allow your incisions to heal and avoid hernias.
Check with your surgeon for their recommendations on when you can start exercise after surgery. Usually, you can start small lower-intensity 10 minute walks within a few days or a week post-op. Keep moving around the house, washing the dishes, light house cleaning and general body movement. Over the next 30 days gradually build your walking time to reach 30-40 minutes non-stop at a light-moderate pace.
Before you start any resistance training with either your body weight or light weights it is a good idea to get medical clearance. Once you are 2 – 4 months post-op aim for 4 or 5 workouts per week, with 3 days of cardio (walking at a moderate pace) and 2 days of resistance training. Resistance training is highly recommended after bariatric surgery to maintain muscle mass, but also to build new muscle which will keep your metabolism firing!
The takeaway.......
Remember, weight loss surgery is not the easy way out.
Your results are directly related to the effort you put in!